what is Abdominal Epilepsy? Symptoms, Causes, Diagnosis, and Treatment Explained
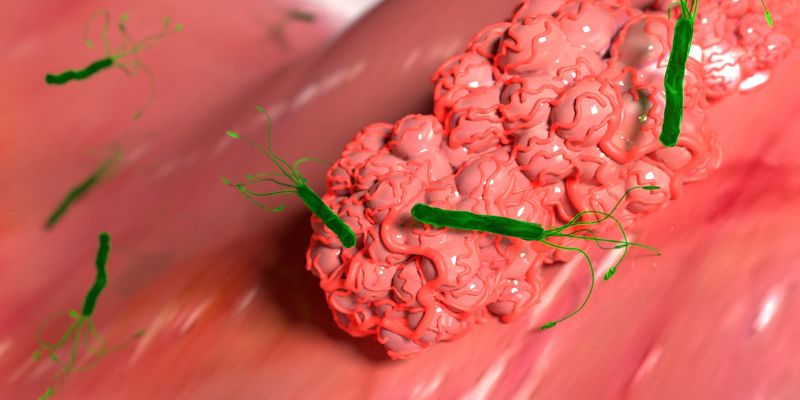
Abdominal epilepsy is a kind of rare epilepsy that mainly strikes the abdomen and digestive systems. Though rarely diagnosed, it may be manifested through seizures involving the abdominal area, usually causing stomach aches, stomach discomfort, and bloating, among others. Since such symptoms mirror other diseases, it has been mistaken as one of these gastrointestinal diseases. The exact cause of abdominal epilepsy is not well understood, but it is associated with abnormal brain activity that influences the digestive system. The following article will explore symptoms, causes, diagnosis, and treatment options for this rare condition.
What is Abdominal Epilepsy?
Abdominal epilepsy is a rare form of epilepsy in which seizures cause unusual activity in the abdominal area. These seizures usually impact the stomach, intestines, and other digestive organs and can lead to symptoms like abdominal pain, bloating, nausea, and discomfort. Because these symptoms are closely related to those of other gastrointestinal disorders, abdominal epilepsy is challenging to diagnose. The seizures may vary in intensity and duration, making them difficult to distinguish from common gastrointestinal complaints, such as irritable bowel syndrome or food intolerances. Accurate diagnosis is very important in successful treatment and management.

Symptoms of Abdominal epilepsy
The symptoms of abdominal epilepsy can often be very mild and are therefore unable to be differentiated from other gastroenterological disorders. One of the common signs it may present is as follows:
- Abdominal Pain: That is the hallmark symptom of abdominal epilepsy. The pain may be sharp, crampy, dull, and aching, and it usually starts without warning.
- Bloating: Sometimes, people experience bloating, a feeling of fullness in the stomach. This symptom causes discomfort and resembles other conditions, such as indigestion or gas.
- Nausea and Vomiting: Intense abdominal pain is associated with nausea and sometimes even vomiting. These symptoms arise mainly because of the intensity of the seizures.
- Altered Bowel Habits: Some people with abdominal epilepsy also suffer from altered bowel movements. Some have diarrhea, while others may experience constipation due to the abnormal brain activities that alter the normal function of the digestive system.
- Loss of Appetite: Stomach ache and bloating that does not subside may trigger a loss of appetite, which will cause weight loss in those suffering from this illness.
Treatment for Abdominal Epilepsy
Though abdominal epilepsy is an extremely rare condition, various treatments can be administered to manage the symptoms and prevent the occurrence of seizures. The treatment generally includes medication, lifestyle modification, and, in some cases, surgery.
Medication
The first-line treatment of abdominal epilepsy is anticonvulsant medications that regulate the seizure activity of the brain. Most antiepileptic drugs (AEDs) used for regulating seizure activities include the use of carbamazepine, valproate, and sometimes topiramate, wherein drugs stabilize electrical functions within the brain. Medication in some instances: the benzodiazepine. Medications like diazepam can be used to give instant relief in the seizure instance and also to stop one's occurrence.
Lifestyle Modifications
Certain lifestyle adjustments may help decrease seizure frequency and improve the quality of life in patients with abdominal epilepsy:
- Stress Management: Stress management through relaxation techniques, such as yoga, meditation, and deep breathing exercises, may help decrease the occurrence of seizures induced by stress or anxiety.
- Healthy Diet: A balanced diet that avoids foods irritating the stomach can help manage gastrointestinal symptoms. Avoiding caffeine and spicy foods is often recommended.
- Regular Sleep Patterns: Getting adequate rest and maintaining regular sleep is crucial in managing epilepsy. Sleep deprivation can trigger seizures in some individuals.
Surgery
In rare cases where medication and lifestyle changes do not effectively control seizures, surgical intervention may be considered. This may include surgery to remove brain tissue causing abnormal electrical activity or deep brain stimulation to regulate brain function.
Psychological Support
Since stress and anxiety could initiate or worsen a seizure, psychological treatment is crucial to this treatment. Through counseling and cognitive behavioral therapy, people can manage the psychological stressors of having such a condition and live better with stress.

Diagnosis of Abdominal Epilepsy
Abdominal epilepsy is difficult to diagnose because its symptoms closely mimic those of many gastrointestinal disorders. A combination of the following approaches is often used by healthcare professionals to diagnose abdominal epilepsy accurately:
- Medical History and Physical Examination
A detailed medical history and physical examination are the initial steps in diagnosing abdominal epilepsy. The health care provider reviews the symptoms, their onset, duration, and frequency. This helps to exclude other potential conditions with similar symptoms, such as irritable bowel syndrome or gastritis. The doctor may also assess a previous history of seizures or neurological disorders.
- EEG (Electroencephalogram)
An EEG is an essential diagnostic tool for epilepsy. This test records electrical activity in the brain. Abnormal brain waves during the test can diagnose a seizure disorder. For abdominal epilepsy, an EEG may show patterns that indicate seizure activity originating from the abdominal area.
- Imaging Tests
One of the structural brain imaging techniques that may be used to rule out the presence of other neurological disorders or structural abnormalities that cause seizures is MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans. These tests help identify any potential lesions in the brain, tumors, or other conditions contributing to the seizures.
- Gastrointestinal Testing
Abdominal epilepsy has symptoms that overlap with many gastrointestinal conditions, so these have to be ruled out. Tests like endoscopy (examining the digestive tract) and stool analysis (infections or digestive issues) are helpful in excluding common gastrointestinal causes. They will confirm that the symptoms are not because of gastritis, peptic ulcers, or inflammatory bowel disease.
Conclusion
It's a rare but significant kind of epilepsy that affects the stomach and digestive system; symptoms, causes, diagnosis, and treatment options are really important for the proper management of the condition. Adequate management of abdominal epilepsy, together with medication, lifestyle adjustments, and psychological support, can better control the condition and even improve the quality of life. When a person doubts the presence of abdominal epilepsy, it is advisable to visit a healthcare provider for the proper diagnosis and treatment.